HYPERCALCEMIA in critically ill patients
HYPERCALCEMIA.
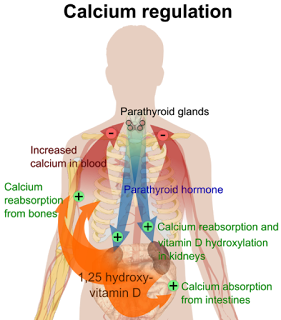
Hypercalcemia is rare in critically ill patients, estimated to be present in between 1% and 15% of ICU patients. Defined as an increase in serum calcium above 10.4 mg/dL (2.60 mmol/L), hypercalcemia usually is caused by excessive bone resorption.
Most common causes:
- Hyperparathyroidism
- Humoral hypercalcemia of malignancy
- Sarcoidosis
- Prolonged immobilization
- Medications (e.g., thiazide diuretics).
Clinical findings:
Mild hypercalcemia is usually asymptomatic. However, patients with circulating Ca2+ above 12 mg/dL may manifest symptoms:
- Neurological: confusion, delirium, psychosis, and coma.
- Gastrointestinal: nausea, vomiting, constipation, abdominal pain and ileus.
- Cardiovascular: hypotension, hypovolemia, and shortened QT interval.
- Profound skeletal muscle weakness may result. Seizures, however, are rare
Management:
The treatment of hypercalcemia should be directed at the underlying medical condition. Saline infusion and diuresis are indicated in symptomatic patients and when the serum calcium level rises above 14 mg/dL (3.5 mmol/L).
For patients with underlying malignancy, treatment with salmon calcitonin, pamidronate, or plicamycin may be necessary. These agents act to inhibit bone resorption.
Hydrocortisone can also be used in combination with calcitonin to treat hypercalcemia associated with multiple myeloma.