Recommendations for perioperative P2Y12 inhibitor management (EACTS).
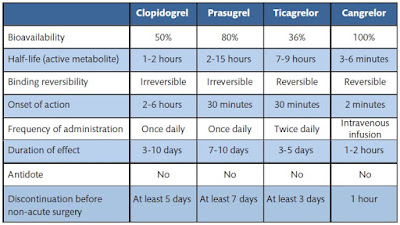
Dual antiplatelet therapy (DAPT) with ASA and P2Y12-receptor inhibitors (clopidogrel, ticagrelor and prasugrel) (Table) reduces the risk for thrombotic complications in patients with acute coronary syndrome (ACS) compared to treatment with ASA only, especially if they undergo percutaneous coronary intervention. The risk for thrombotic
complications is further reduced if one of the more potent third-generation P2Y12 inhibitors (ticagrelor or prasugrel) is used instead of clopidogrel, at the expense of increased spontaneous and surgical bleeding complications.
complications is further reduced if one of the more potent third-generation P2Y12 inhibitors (ticagrelor or prasugrel) is used instead of clopidogrel, at the expense of increased spontaneous and surgical bleeding complications.
Discontinuation before surgery.
Continuing DAPT until the operation increases the risk of bleeding, transfusions and reexploration for bleeding, as shown in RCTs, observational studies and meta-analyses. It is, therefore, recommended that P2Y12-receptor inhibitors be discontinued before elective surgery whenever possible. Alternatively, elective operations may be postponed until the DAPT treatment period is completed. In urgent cases—most often in patients with ACS—the risk for thromboembolic episodes (stent thrombosis and MI) while waiting for the effect of the P2Y12-receptor inhibitors to cease must be weighed against the risk for perioperative bleeding complications.
In patients who are at extreme high risk for thrombotic events, e.g. recent stent implantation, bridging therapy may be considered or surgery may be performed without discontinuation of P2Y12 inhibitors. If bridging is warranted, GPIIb/GPIIIa inhibitors may be used. However, cangrelor, a new reversible intravenous P2Y12 inhibitor with an ultrashort half-life, has demonstrated a high rate of maintenance for platelet inhibition and no excessive perioperative bleeding complications. Safe discontinuation intervals differ according to the pharmacodynamics and pharmacokinetic profile of each P2Y12-receptor inhibitor. When P2Y12-receptor inhibitors are discontinued, ASA therapy should be continued until the operation.
Discontinuation of clopidogrel 5 days or more before CABG did not increase the risk for bleeding complications. A longer time interval (7 days) is recommended for prasugrel due to the longer offset of platelet inhibition and a higher incidence of CABG-related bleeding complications compared with that for clopidogrel. In patients treated with ticagrelor, discontinuation of the drug 3 to 4 days, as opposed to 5 days or more before CABG surgery, is not associated with a higher incidence of bleeding complications (OR 0.93; 95% CI 0.53 1.64, P = 0.80).
This finding has been confirmed in multiple studies. It is unlikely that the optimal discontinuation period before surgery of any of the P2Y12 inhibitors will ever be tested in an RCT with clinically relevant end points.
Restart after surgery.
Current guidelines recommend DAPT for all patients with ACS independently of revascularization treatment. This recommendation also applies to patients having CABG or other non-coronary cardiac operations.
Furthermore, DAPT after CABG has been associated with reduced all-cause mortality and better vein graft patency (OR 0.59; 95% CI 0.43–0.82), although the evidence is conflicting.
Furthermore, DAPT after CABG has been associated with reduced all-cause mortality and better vein graft patency (OR 0.59; 95% CI 0.43–0.82), although the evidence is conflicting.
The potential benefits of DAPT after CABG are offset by increased risk for bleeding complications.
The magnitude of the benefit, i.e. a reduction in the mortality rate of more than 50% , appears to be more pronounced in patients with ACS than in those with stable angina and with P2Y12 inhibitors that are more potent than clopidogrel. It is recommended to restart DAPT after CABG as soon as it is considered safe in patients with ACS. There is currently no evidence to support starting routine DAPT after CABG in patients not receiving DAPT preoperatively, although starting DAPT may be considered in patients with a higher ischaemic risk due to a coronary endarterectomy or off-pump surgery. The optimal timing for restarting should be as soon as it is deemed safe. In patients with a high risk of ischaemia, P2Y12 inhibitors should be restarted within 48 h after surgery. In contrast, it may be considered safe to reinitiate P2Y12 inhibitors 3–4 days postoperatively when the risk for ischaemia is low (e.g. recent stent implantation > 1 month or ACS without stenting).
Stay tuned! Sign up with Facebook!