DIAGNOSTIC CRITERIA AND CLINIC SIGNS OF ARDS
Acute respiratory distress syndrome (ARDS) is a clinical syndrome of severe dyspnea of rapid onset, hypoxemia, and diffuse pulmonary infiltrates leading to respiratory failure.
Assosiated disorders and causes:
DIRECT LUNG INJURY:
- Pneumonia
- Aspiration of gastric contents
- Pulmonary contusion
- Near-drowning
- Toxic inhalation injury
INDIRECT LUNG INJURY:
- Sepsis
- Severe trauma
- Multiple bone fractures
- Flail chest
- Head trauma
- Burns
- Multiple transfusions
- Drug overdose
- Pancreatitis
- Postcardiopulmonary bypass
Diagnostic Criteria for ARDS:
SEVERITY: OXYGENATION:
- Mild: 200 mmHg < PaO2 /FiO2 ≤ 300 mmHg
- Moderate: 100 mmHg < PaO2 /FiO2 ≤ 200 mmHg
- Severe: PaO2 /FiO2 ≤ 100 mmHg
ONSET:
Acute: Within 1 week of a clinical insult or new or worsening respiratory symptoms.
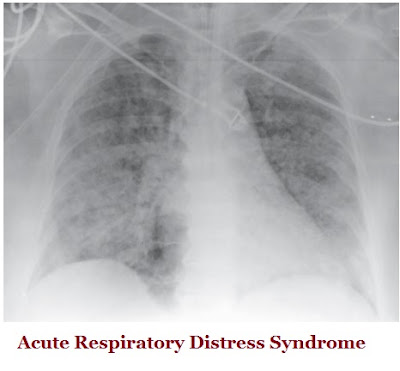
CHEST RADIOGRAPH:
Bilateral opacities consistent with pulmonary edema not fully explained by effusions, lobar/lung collapse, or nodules
ABSENCE OF LEFT ATRIAL HYPERTENSION:
Hydrostatic edema is not the primary cause of respiratory failure. If no ARDS risk factor is present, then some objective evaluation is required (e.g., echocardiography) to rule out hydrostatic edema
Phases of ARDS:
Radiographic findings are not specific and can be indistinguishable from cardiogenic pulmonary edema. But chest x-ray in ARDS may not demonstrate cardiomegaly, pleural effusions, or pulmonary vascular redistribution as is often present in pure cardiogenic pulmonary edema.
Lasts from day 7 to day 21. Despite improvement,
many patients still experience dyspnea, tachypnea, and hypoxemia. Some patients develop progressive lung injury and early changes of pulmonary fibrosis. Type II pneumocytes proliferate along alveolar basement membranes. These specialized epithelial cells synthesize new pulmonary surfactant and differentiate into type I pneumocytes.
While many patients with ARDS recover lung function 3–4 weeks after the initial pulmonary injury, some enter a fibrotic phase that may require long-term support on mechanical ventilators and/or supplemental oxygen. The physiologic consequences include an increased risk of pneumothorax, reductions in lung compliance, and increased pulmonary dead space.
Phases of ARDS:
I. EXUDATIVE PHASE:
Alveolar capillary endothelial cells and type I pneumocytes are injured, with consequent loss of the normally tight alveolar barrier. Edema fluid that is rich in protein accumulates in the interstitial and alveolar spaces. Condensed plasma proteins aggregate in the air spaces with cellular debris and dysfunctional pulmonary surfactant to form hyaline membrane whorls. Collapse of large sections of dependent lung can contribute to decreased lung compliance and with diminished aeration. Although usually presenting within 12–36 h after the initial insult, symptoms can be delayed by 5–7 days. Dyspnea develops, with a sensation of rapid shallow breathing and an inability to get enough air. Tachypnea and increased work of breathing result frequently in respiratory fatigue and ultimately in respiratory failure.
II. PROLIFERATIVE PHASE
many patients still experience dyspnea, tachypnea, and hypoxemia. Some patients develop progressive lung injury and early changes of pulmonary fibrosis. Type II pneumocytes proliferate along alveolar basement membranes. These specialized epithelial cells synthesize new pulmonary surfactant and differentiate into type I pneumocytes.
III. FIBROTIC PHASE
While many patients with ARDS recover lung function 3–4 weeks after the initial pulmonary injury, some enter a fibrotic phase that may require long-term support on mechanical ventilators and/or supplemental oxygen. The physiologic consequences include an increased risk of pneumothorax, reductions in lung compliance, and increased pulmonary dead space.