Preload
Preload represents the stretch on the muscle just prior to its contraction. Preload in the intact heart is influenced by a number of factors that impact on ventricular filling (and hence end-diastolic stretch). These factors include:
- blood volume,
- venous capacitance,
- ventricular compliance,
- atrial function,
- valvular function,
- heart rate.
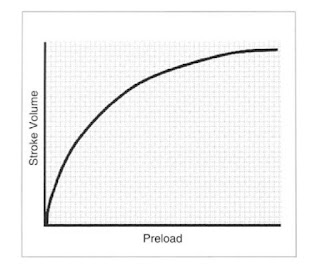
The Frank-Starling relationship demonstrates increasing stroke volume
with increasing preload. Notice that stroke volume is more sensitive to changes in
preload at low values compared to high values:
How do we estimate preload clinically? With the widespread use of
transesophageal echocardiography (TEE), it is possible to get a reasonable
estimate of chamber size and, hence, preload. In the absence of
TEE, we substitute the pressure at end-diastole with the assumption
that the higher the pressure, the greater the size and the greater the
stretch on the contractile elements . EDP can be assessed clinically by
measuring the pulmonary capillary wedge pressure (PCWP) using a
Swan-Ganz catheter that is placed through the right ventricle (RV) into
the pulmonary artery (PA). When the balloon at the tip of the
catheter is inflated, it occludes flow in that small branch of the PA; the
pressure distal to the balloon quickly equilibrates with the pressure in
the pulmonary venous system. As the risk of pulmonary rupture and
hemorrhage is increased with anticoagulation, the pulmonary arterial
diastolic pressure is often used instead of the PCWP. In the absence of
a PA catheter, central venous pressure is used to assess volume status
with the assumption that there is a positive association between changes
in central venous pressure and LV size.
(On Bypass : Advanced Perfusion Techniques, edited by Linda B. Mongero)
Normal:
Pulmonary capillary wedge pressure 2-15 mmHg
Pulmonary artery pressure sys. 15 - 30 mmHg, diast 4-12 mmHg
Central venous pressure 3-8 mmHg