Cardiac Arrest. Shockable and Non-Shockable Rhythms
Cardiac Arrest. Shockable and Non-Shockable Rhythms
keywords: cardiac arrest, shockable rhythm, non-shockable rhythm, defibrillation, CPR, heart rhythm, ventricular fibrillation, asystole, emergency medicine, resuscitation
Acute restoration of sinus rhythm.
Cardiac arrest is a sudden stop in effective blood flow due to the failure of the heart to contract effectively.
During cardiopulmonary resuscitation (CPR) it is obligatorily to recognize Shockable or Non-Shockable the heart rhythm. It is important to know when to use defibrillation.
Shockable Rhythms:
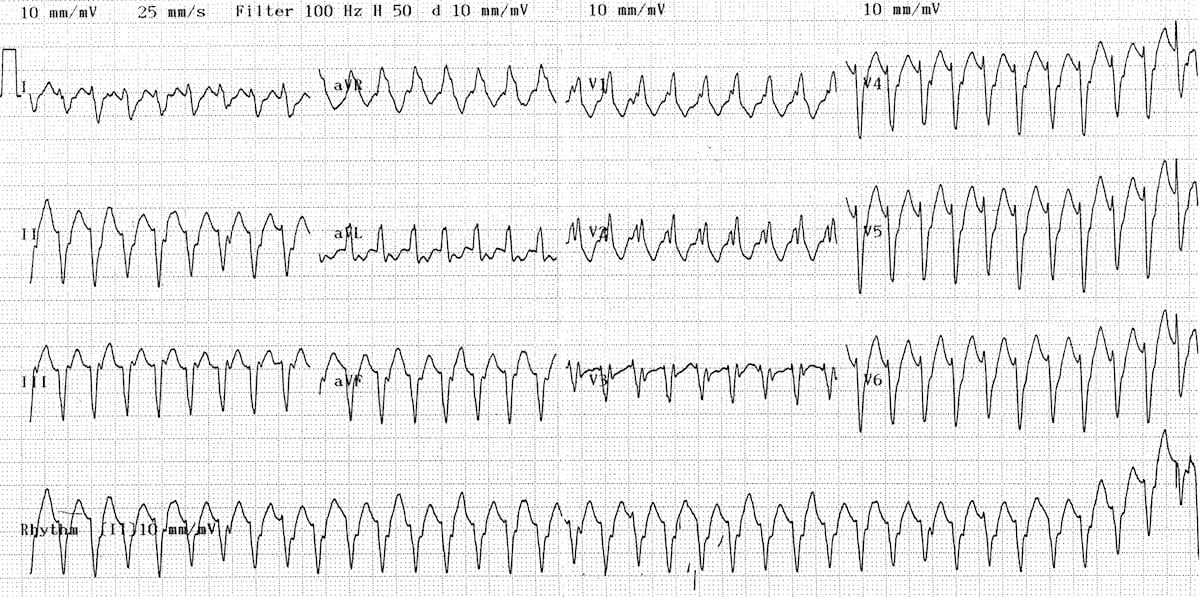
Ventricular Tachycardia
Ventricular tachycardia (often shortened to v-tach) appears on the monitor as a wide, regular, and very rapid rhythm. Ventricular tachycardia is a poorly perfusing rhythm; patients may present with or without a pulse. Most patients are unconscious and pulseless with this rhythm and defibrillation is needed to ‘stun’ the heart so that the primary pacemaker (usually the S-A node) can take over. Multiple shocks may be needed, but good compressions and adequate ventilation are also important.
Ventricular fibrillation, or v-fib,on the monitor will look like a frenetically disorganized wavy line. Ventricular fibrillation may be fine or coarse; coarse ventricular fibrillation is more likely to convert after defibrillation than fine v-fib. Fine v-fib is sometimes mistaken for asystole. As the treatments for asystole and ventricular fibrillation are different, it is important to differentiate between the two. If in doubt, it is acceptable to deliver a shock. If it is fine v-fib, you may terminate the rhythm; however, if the rhythm is asystole, defibrillation will be ineffective and you can follow the asystole protocol with confidence.
Supraventricular tachycardia, or SVT, is far different than the rhythms discussed above, which originate in the ventricles. Patients in a supraventricular tachycardia will have a rapid rhythm with a heart rate greater than 150 beats per minute. The patient with an SVT may be relatively stable with few symptoms or profoundly unstable with severe signs and symptoms related to the rapid heart rate. Patients who are unstable or who do not respond to medication will require electrical therapy. In this case, synchronized cardioversion, rather than defibrillation, is performed. If the patient is conscious sedation should be provided, as cardioversion is painful. The shock that is delivered in cardioversion for SVT is synchronized to occur at a precise time, one that avoids the vulnerable refractory period which could cause ventricular fibrillation. Smaller doses of energy are needed to convert SVTs such as atrial fibrillation and atrial flutter.
Non-Shockable Rhythms:
In PEA, the monitor will show electrical activity in the heart, but the patient will have no palpable pulse. its most frequent causes are hypovolemia and hypoxemia. Patients may have weak ventricular contractions and recordable aortic pressure (pseudo-PEA). True PEA is a condition in which cardiac contractions are absent in the presence of coordinated electrical activity. Measure QRS duration, since it has prognostic significance. Patients with QRS duration of less than 0.2 second are more likely to recover, and high-dose epinephrine may be administered.
Asystole is also known as flatline. It is a state of cardiac standstill with no cardiac output and no ventricular depolarization.