Spinal Opioid Dosages for Labor and Delivery.
Spinal Opioid Dosages for Labor and Delivery: A Guide for Anesthesiologists
Keywords: spinal opioid dosages, labor and delivery analgesia, epidural vs spinal anesthesia, intrathecal opioids, pain management in labor
Pain management during labor and delivery is a cornerstone of obstetric anesthesiology. Among the most effective techniques is the use of spinal opioid dosages, often administered via intrathecal injection as part of a combined spinal-epidural (CSE) or standalone spinal anesthesia. These methods provide rapid, targeted pain relief with minimal systemic side effects. In 2025, advancements in dosing protocols and opioid selection have refined their use, making them a go-to choice for labor analgesia. This article explores the latest recommendations for spinal opioid dosages in labor and delivery, their benefits, risks, and practical tips for anesthesiologists aiming to optimize maternal outcomes.
Why Spinal Opioids Are Key in Labor Analgesia
Labor pain is intense, driven by uterine contractions and cervical dilation, and progresses to somatic pain during delivery. Spinal opioids, such as fentanyl, sufentanil, and morphine, target opioid receptors in the spinal cord’s dorsal horn, offering rapid analgesia without the motor blockade associated with higher doses of local anesthetics. When combined with techniques like epidural anesthesia, they enhance pain control while allowing mothers to remain active during labor.
The appeal of intrathecal opioids lies in their speed and precision. Unlike systemic opioids, spinal administration minimizes neonatal sedation and maternal side effects like respiratory depression, making them ideal for labor and delivery pain management. But what dosages work best, and how should they be applied? Let’s dive into the evidence.
Recommended Spinal Opioid Dosages for Labor
Dosages vary based on the opioid’s lipophilicity (how quickly it acts and clears) and the clinical context (e.g., early labor vs. cesarean delivery). Below are the most current recommendations for spinal opioid dosages in labor analgesia, based on 2025 guidelines from the American Society of Anesthesiologists (ASA) and recent studies:
- Fentanyl
- Dosage: 10-25 µg intrathecally
- Onset: 5-10 minutes
- Duration: 1-2 hours
- Use Case: Ideal for early labor or as part of a CSE. Its lipophilic nature ensures quick pain relief with a short duration, perfect for dynamic labor stages.
- Evidence: A 2024 study in Anesthesiology showed 15 µg fentanyl reduced pain scores by 80% within 10 minutes, with no significant fetal impact.
- Sufentanil
- Dosage: 2.5-7.5 µg intrathecally
- Onset: 5-10 minutes
- Duration: 2-4 hours
- Use Case: Preferred for longer-lasting analgesia, such as late labor or postpartum pain control. Its higher potency requires lower doses.
- Evidence: Research in Regional Anesthesia & Pain Medicine (2025) found 5 µg sufentanil superior to fentanyl for sustained relief without increased side effects.
- Morphine
- Dosage: 0.1-0.25 mg intrathecally
- Onset: 15-30 minutes
- Duration: 6-12 hours
- Use Case: Best for post-cesarean analgesia rather than active labor, due to its slower onset and prolonged effect.
- Evidence: A 2023 meta-analysis confirmed 0.2 mg morphine reduces opioid needs post-cesarean by 40% over 24 hours.
- Combined with Local Anesthetics
- Adding bupivacaine (2.5-5 mg) or ropivacaine (2-4 mg) to spinal opioids enhances analgesia while reducing opioid doses, minimizing side effects like pruritus or nausea.
(Looking for more labor analgesia tips? Check out our guide on epidural techniques!)
Benefits of Spinal Opioids in Labor and Delivery
When dosed correctly, spinal opioids offer distinct advantages:
- Rapid Pain Relief: Intrathecal administration bypasses systemic circulation, acting directly on spinal receptors.
- Minimal Motor Block: Unlike high-dose local anesthetics, opioids preserve maternal mobility, aiding natural delivery.
- Reduced Neonatal Impact: Low transfer to the fetus compared to IV opioids ensures safer outcomes.
- Flexibility: Easily paired with epidural anesthesia for continuous pain control throughout labor and delivery.
A 2025 trial in Obstetric Anesthesia Digest reported that CSE with 15 µg fentanyl shortened the first stage of labor by 20% compared to epidural-only techniques, highlighting its efficacy.
Risks and Side Effects to Watch For
While effective, spinal opioid dosages aren’t without risks:
- Pruritus: Common with fentanyl and sufentanil (up to 50% incidence), though typically mild.
- Nausea: Seen in 10-20% of cases, manageable with antiemetics like ondansetron.
- Respiratory Depression: Rare with lipophilic opioids (<1%), but a concern with morphine, requiring monitoring for 12-24 hours post-dose.
- Fetal Bradycardia: Linked to rapid pain relief altering catecholamine levels; incidence is 8-10% with CSE, per a 2024 review.
Anesthesiologists must weigh these risks against benefits, tailoring dosages to patient needs and monitoring closely.
Practical Tips for Administering Spinal Opioids
Here’s how to optimize spinal opioid use in labor and delivery:
- Timing: Administer fentanyl or sufentanil early in labor (3-4 cm dilation) for maximum effect; reserve morphine for post-delivery analgesia.
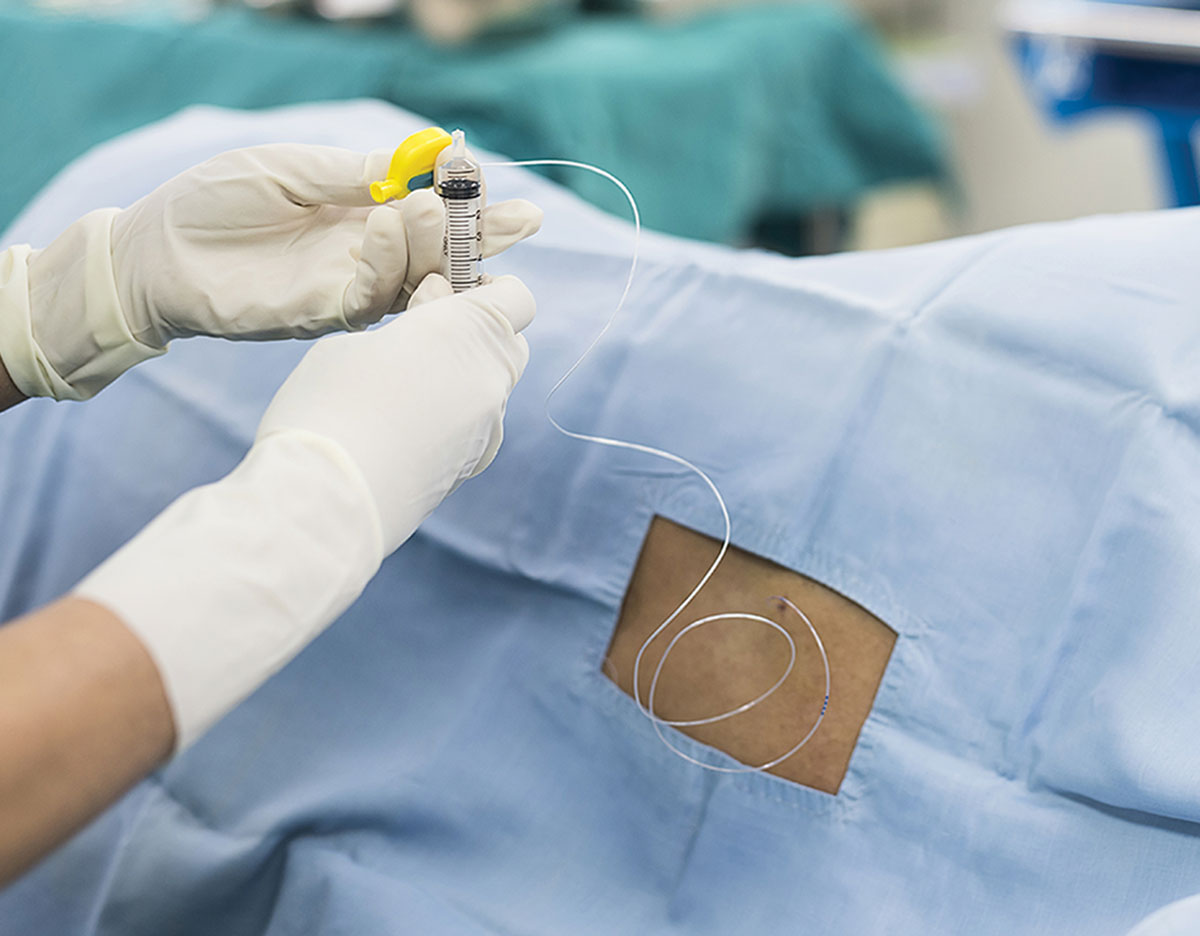
- Technique: Use a CSE approach—place the spinal dose, then thread an epidural catheter for flexibility.
- Monitoring: Check respiratory rate and oxygen saturation every 1-2 hours post-morphine; less frequent with fentanyl/sufentanil.
- Patient Education: Inform mothers about potential itching or nausea to reduce anxiety.
(Need more anesthesiology insights? Subscribe to our blog for expert updates!)
Epidural vs. Spinal Opioids: What’s the Difference?
While spinal opioids provide fast, targeted relief, epidural anesthesia offers continuous dosing via a catheter. Combining them in a CSE leverages both strengths:
- Spinal: Quick onset, ideal for acute pain spikes.
- Epidural: Adjustable, suited for prolonged labor or cesarean delivery.
A 2025 study in Journal of Clinical Anesthesia found CSE reduced total opioid use by 30% compared to epidural alone, enhancing safety.
Future Trends in Spinal Opioid Use
Research is evolving:
- Lipid-Soluble Innovations: Newer opioids with shorter durations are in trials.
- Adjuncts: Clonidine or dexmedetomidine may further reduce opioid needs.
- Personalized Dosing: Genetic profiling could soon guide dosages for optimal efficacy.
Stay ahead by following these developments in obstetric analgesia!
Conclusion
Spinal opioid dosages are a powerful tool for labor and delivery analgesia, balancing rapid pain relief with maternal and fetal safety. Fentanyl (10-25 µg) and sufentanil (2.5-7.5 µg) excel in active labor, while morphine (0.1-0.25 mg) shines post-cesarean. By mastering these protocols, anesthesiologists can elevate patient care and satisfaction. Have experiences or questions about intrathecal opioids? Share them in the comments below!
(Explore more pain management strategies on our blog!)