Management of Dyslipidemias 2019, Lipid Guidelines
The following are key points to remember from the 2019 European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) guidelines for the management of dyslipidemias: lipid modification to reduce cardiovascular (CV) risk:
- Lipid guidelines aimed at reducing risk of atherosclerotic CV disease (ASCVD) have been issued in recent years by ESC and jointly by the American College of Cardiology and American Heart Association. The topics addressed by the European and US expert teams are similar, but conclusions often differ. Not uncommonly, the differences are related to the regions and populations from which the recommendations are derived and the cost/value implications of the decisions. The approach herein will be to present the new ESC/EAS recommendations. This 2019 European guideline is similar to the most recent US guideline for prevention of ASCVD. The focus will be on risk estimates and lipids and differences will be described.
- The European prevention strategies for ASCVD are based on total CVD risk with intensity proportionate to risk. The European SCORE (Systematic Coronary Risk Estimation) system is recalibrated for high-risk versus low-risk regions of Europe. Risk factors include age, sex, systolic blood pressure (SBP), high-density lipoprotein cholesterol (HDL-C), and total cholesterol with BP and cholesterol preferably baseline. It estimates 10-year risk of CV deaths and estimates a threefold fixed multiplier for ASCVD events.
- In the European guideline, all persons are recommended diet with low saturated fat, high in fiber and fish; target body mass index 20-25 kg/m2; waist < 37 inches in men and 31.4 inches in women; 3.5-7 hours of moderate physical activity per week or 30-60 minutes most days. Goal for diabetes is a hemoglobin A1c of < 7% as in US (ADA < 6.5%), and BP < 140/90 mm Hg, while the US goal is < 130/80 mm Hg.
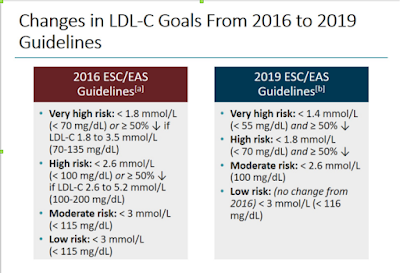
- Unlike the US guideline that recommends high- or intermediate-intensity statins with intensifying for acute coronary syndrome (ACS) and very high risk by risk enhancers, the 2019 European version returned to low-density lipoprotein cholesterol (LDL-C) cut-points. The European guideline recommends a high-intensity statin up to the highest tolerated dose to reach target goals for specific levels of risk. Very high-risk includes documented ASCVD (any clinical CVD/event or imaging), diabetes with end-organ damage, or three major risk factors, severe chronic kidney disease (CKD) (estimated glomerular filtration rate [eGFR] < 30), heterozygous familial hypercholesterolemia (HeFH) with ASCVD or another major risk factor, or a SCORE ≥ 10% (e.g., annual CV death ≥1%) in which the LDL-C target is ≥ 50% reduction in LDL-C with goal < 55 mg/dl. High risk is a very high single risk factor (total cholesterol > 310 mg/dl, LDL-C > 190 mg/dl, BP 180/110 mm Hg), diabetes > 10 years or with one major risk factor, moderate CKD (eGFR 30-59), or SCORE 5-9% in which target LDL-C is < 70 mg/dl. Moderate risk is a SCORE 1-4%, which is not uncommon, and includes type 1 diabetes mellitus (T1DM) < 35 years, type 2 diabetes mellitus (T2DM) < 50 years without other risk factors in which target LDL-C < 100 mg/dl, and low risk a SCORE of < 1% where a goal of < 116 mg/dl should be considered.
- The ESC/EAS uses the term risk modifiers that are similar but more extensive than US risk enhancers and related to increase in CV deaths and not simply ASCVD events. These include social deprivation, major psychological disorders, lower socioeconomic status, physical inactivity, CKD, obstructive sleep apnea, left ventricular hypertrophy, and atrial fibrillation. As in the US guideline, for those at moderate risk, several other factors may improve risk classification including increased apolipoprotein B, lipoprotein a [Lp (a)], triglycerides, C-reactive protein, and plaque in the carotid or femoral arteries or the coronary artery calcium (CAC) score. Zero score infers low risk and CAC > 100 high risk.
- SCORE estimates 10-year cumulative risk of a fatal ASCVD event in contrast to the US Pooled Cohort Equation (US-PCE), which estimates 10-year risk of a first ASCVD. The European use of CV mortality rather than first ASCVD is preferred because it provides a definite endpoint in contrast to CV events that vary by definitions, severity, diagnostic tests, each of which limit the ability to relate fatal to total events. Total CVD event risk is about 3x higher than risk for fatal CVD or a risk of 5% fatal translates into 15% risk of fatal + nonfatal CVD events; the multiplier is higher in women and lower in the elderly. Using the SCORE from low-risk regions of Europe, a 60-year-old man, nonsmoker, SBP 140 mm Hg, and total cholesterol 210 mg/dl has a 10-year CV mortality of 3, a score considered moderate. Using the US-PCE ASCVD Risk Estimator Plus, the 10-year risk of an ASCVD event is 11.3%. Both Europe and US guidelines recommend a statin, with Europe having a target of < 100 mg/dl, the US a moderate-intensity statin, and each recommending considering lipid and other enhancers.
- European guideline: For primary prevention in HeFH patients who are at very high risk, an LDL-C reduction of ≥50% from baseline and an LDL-C goal of < 55 mg/dl should be considered. For US guideline: Patients 30-75 years of age with HeFH and with an LDL-C level of 100 mg/dl ( ≥ 2.6 mmol/L) or higher while taking maximally tolerated statin and ezetimibe therapy, the addition of a PCSK9 inhibitor may be considered. It would not be necessary if a CAC score is 0 and plans to repeat within 4-5 years with intention to maximize LDL-C lowering with any CAC. The risk estimate is not useful with very high LDL-C. The US-PCE data are not calibrated for differences between an LDL-C of 190 mg/dl and 250 mg/dl. A 25-year-old man with no risk factors and not on treatment with an LDL-C of 250 mg/dl or LDL-C of 190 mg/dl has the same high 50% lifetime risk of ASCVD. Only 2% of those with LDL-C at 190 mg/dl have HeFH, but they have a fourfold risk of ASCVD events at the same LDL-C level, providing rationale for identifying them and intensifying treatment.
- European guideline: Treatment of dyslipidemias with statins is recommended for older persons, according to the risk level, in those age ≤ 75 years. Initiation of statin treatment for primary prevention in older people aged ≥ 75 years may be considered if at high risk or above. US guideline: The decision algorithm regarding statins should not change in the elderly who have a life expectancy of ≥ 5 years.
- European guideline: In very high or high-risk patients with triglycerides between 135-499 mg/dl despite statin treatment, n-3 polyunsaturated fatty acids (PUFAs) (icosapent ethyl 2 x 2 g/day) should be considered in combination with statins. US guideline: Recognizes the value of n-3 PUFAs in high-risk persons defined as ASCVD or diabetes, but suggests either icosapent ethyl or combination EPA/DHA 2 x 2 g/day.
- European guideline: In patients with T2DM at very high risk, an LDL-C reduction of ≥ 50% from baseline and a goal of < 55 mg/dl is recommended. In patients with T2DM at high risk, an LDL-C reduction of ≥50% from baseline and an LDL-C goal of < 70 mg/dl is recommended. Intensification of statin therapy should be considered before introduction of combination therapy. If the goal is not reached, statin combination with ezetimibe should be considered. Statins are recommended in patients with T1DM who are at high or very high risk. Statins are not recommended in premenopausal women with T2DM who are considering pregnancy or not using adequate contraception. US guideline: Diabetics 40-75 years of age and an LDL-C level of ≥ 70 mg/dl, regardless of estimated 10-year ASCVD risk, start moderate-intensity statins. In T2DM at higher risk, especially those with multiple risk factors or those 50-75 years of age, it is reasonable to use a high-intensity statin to reduce the LDL-C level by ≥ 50%.
- European guideline: For patients with an ACS, in whom LDL-C levels are not already at goal despite maximally tolerated statin and ezetimibe, adding a PCSK9 inhibitor early after the event (if possible, during hospitalization for the ACS event) should be considered. For those placed on maximal LDL-C lowering therapy uring the ACS, if LDL-C goal is not achieved in 4-6 weeks despite maximal tolerated statin and ezetimibe, addition of a PCSK9 inhibitor is recommended. US guideline: Recent ACS within 12 months is considered very high risk in which a threshold of LDL-C > 70 mg/dl would indicate adding ezetimibe. Adding a PCSK9 inhibitor is reasonable. Unlike in Europe, adding a PCSK9 inhibitor in the hospital is not feasible because of time to obtain approval from insurance carrier.
- The extensive discussion of the rationale for the new ESC guideline is easily readable and supportive based but for the LDL-C cut-points. Use of the cards and table guideline for the providers seems very difficult unless one uses the internet-based SCORE, which also provides treatment decisions as does the US-PCE ASCVD +. The US-later has been shown to overestimate ASCVD event risk in women and men, particularly those well-educated and with a higher socioeconomic status inferring less at-risk behavior. The ESC 10-year CV death estimate has been shown to underestimate overall CV risk or risk events such as ACS, coronary artery bypass grafting, surgery for vascular disease, and stroke, which are related to quality of life, disability, and cost/benefit. In the Norfolk, England cohort of the European Prospective Investigation of Cancer and Nutrition, using CVD mortality to estimate total CVD risk leads to serious underestimation of risk, particularly in younger age groups, and particularly in women (JØrstad HT, et al., BMJ 2015).