COVID-19: lung ultrasonography
lung ultrasonography
technique
- In order to achieve sensitivity, a thorough lung examination is needed (taking a “lawnmower” approach, attempting to visualize as much lung tissue as possible).
- A linear probe may be preferable for obtaining high-resolution images of the pleural line (to make the distinction between a smooth, normal pleural line versus a thickened and irregular pleural line).
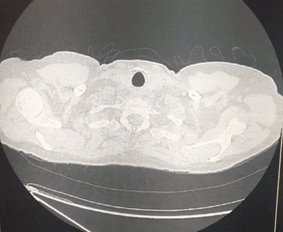
- COVID-19 typically creates patchy abnormalities on CT scan. These will be missed unless ultrasonography is performed overlying the abnormal lung tissue.
findings
- The findings on lung ultrasonography appear to correlate very well with the findings on chest CT scan.
- With increasing disease severity, the following evolution may be seen (Peng 2020)
- (A) Least severe: Mild ground-glass opacity on CT scan correlates to scattered B-lines.
- (B) More confluent ground-glass opacity on CT scan correlates to coalescent B-lines (“waterfall sign”).
- (C) With more severe disease, small peripheral consolidations are seen on CT scan and ultrasound.
- (D) In the most severe form, the volume of consolidated lung increases.
Image of these patterns here.
- Other features:
- Peripheral lung abnormalities can cause disruption and thickening of the pleural line.
- Areas of normal lung (with an A-line pattern) can be seen early in disease, or during recovery.
- Tiny pleural effusions may be seen, but substantial pleural effusions are uncommon (Peng 2020).
- As with CT scans, abnormalities are most common in the posterior & inferior lungs.
- For excellent examples of the correlation between CT scan and lung ultrasonography see Huang et al.
performance
- Sensitivity of lung ultrasonography isn't clearly defined.
- Sensitivity will depend on several factors (most notably disease severity, presence of obesity, and thoroughness of scanning).
- My guess is that a thorough ultrasound exam might have a sensitivity somewhere between CT scanning and chest X-ray (e.g., perhaps sensitivity ~75%?)(Huang et al.). There isn't solid data yet, but it's probably reasonable to extrapolate from our experiences regarding other types of pneumonia.
- Specificity is extremely low. A patchy B-line or consolidation pattern can be seen in any pneumonia or interstitial lung disease. Thus, clinical correlation is necessary (e.g., evaluation of prior chest imaging studies to see if chronic abnormalities are present).
- Note that supine, hospitalized patients may have B-lines and consolidation in a posterior and inferior distribution due to atelectasis. Thus, the lung ultrasonography may have greatest sensitivity and specificity among ambulatory patients.
general approach to imaging
all imaging modalities are nonspecific
- All of the above techniques (CXR, CT, sonography) are nonspecific. Patchy ground-glass opacities may be caused by a broad range of disease processes (e.g. viral and bacterial pneumonias). For example, right now in the United States, someone with patchy ground-glass opacities on CT scan would be much more likely to have a garden variety viral pneumonia (e.g. influenza or RSV) rather than COVID-19.
- Imaging cannot differentiate between COVID-19 and other forms of pneumonia.
- Imaging could help differentiate between COVID-19 and non-pulmonary disorders (e.g. sinusitis, non-pulmonary viral illness).
- Ultimately, the imaging is only one bit of information which must be integrated into clinical context.
possible approach to imaging in COVID-19
- Below is one possible strategy to use for patients presenting with respiratory symptoms and possible COVID-19.
- The temptation to get a CT scan in all of these patients should be resisted. In most cases, a CT scan will probably add little to chest X-ray and lung ultrasonography (in terms of actionable data which affects patient management).
- From a critical care perspective, CT scanning will likely add little to the management of these patients (all of whom will have diffuse infiltrates).
Schema for imaging patients with respiratory symptoms and suspected COVID-19.
additional information:
- RSNA focus page on coronavirus (contains fantastic slide show that provides an appreciation of possible imaging findings in a few minutes)