Dead space of the respiratory system
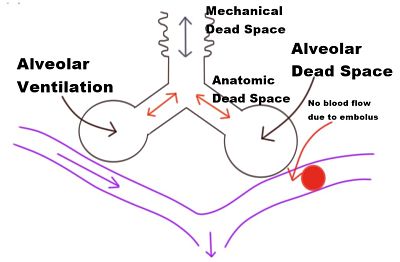
Dead space is the volume of inspired air that takes no part in gas exchange.
Divided into 2 parts:
◗ anatomical dead space: mouth, nose, pharynx and large airways not lined with respiratory epithelium.
◗ alveolar dead space: unperfused alveoli. Ventilated lung normally contributing to gas exchange, but not doing so because of impaired perfusion. Thus represents one extreme of V̇/Q̇ mismatch.
Physiological dead space equals anatomical plus alveolar dead space. It is calculated using the Bohr equation. Assessment may be useful in monitoring V̇/Q̇ mismatch in patients with extensive respiratory disease, especially when combined with estimation of shunt fraction. Normally equals 2–3 ml/kg; i.e., 30% of normal tidal volume. In rapid shallow breathing, alveolar ventilation is reduced despite a normal minute ventilation, because a greater proportion of tidal volume is dead space.
• Increased by:
◗ increased lung volumes.
◗ bronchodilatation.
◗ neck extension.
◗ PE/gas embolism.
◗ old age.
◗ hypotension.
◗ haemorrhage.
◗ pulmonary disease.
◗ general anaesthesia and IPPV.
◗ atropine and hyoscine.
◗ apparatus (see later).
• Decreased by:
◗ tracheal intubation and tracheostomy.
◗ supine position.
Apparatus dead space represents ‘wasted’ fresh gas within anaesthetic equipment. Minimal lengths of tubing should lie between the fresh gas inlet of a T-piece and the patient, especially in children, whose tidal volumes are small.
Facemasks and their connections may considerably increase dead space.