Thalassemia
Thalassemia is a hereditary underproduction of either the alpha or beta globin chains of the hemoglobin molecule, resulting in a hypochromic, microcytic anemia. Gene deletion results in variable levels of disease. There are 4 genes coding for the alpha chain of hemoglobin.
There can be deletions of 1, 2, 3, or all 4 genes:
• Beta thalassemia can be mutated in either 1 or 2 genes.
• Alpha thalassemia is more common in Asian populations, while beta thalassemia is more common in Mediterranean populations.
Clinical Presentation. Presentation depends on the number of abnormal genes.
• Alpha thalassemia
– – 1 gene deletion yields a normal patient; CBC (complete blood count), hemoglobin, and MCV (mean corpuscular volume) are normal.
– – 2 gene deletion yields a mild anemia with hematocrit 30–40% and strikingly low MCV.
– – 3 gene deletion yields a more profound anemia with hematocrit 22–32% and very low MCV.
– – 4 gene deletion alpha thalassemia causes patients to die in utero, secondary to gamma chain tetrads called hemoglobin Barts.
• In beta thalassemia trait there is a mild anemia with marked microcytosis (low MCV).
– – Patients with beta thalassemia major (or Cooley’s anemia) are homozygous for mutations of both genes coding for the beta hemoglobin gene. Patients become severely symptomatic starting age 6 months, when the body would normally switch from fetal hemoglobin to adult hemoglobin. They are severely symptomatic with growth failure, hepatosplenomegaly, jaundice, and bony deformities secondary to extramedullary hematopoiesis. They are later symptomatic from hemochromatosis, cirrhosis, and CHF from chronic anemia and transfusion dependence.
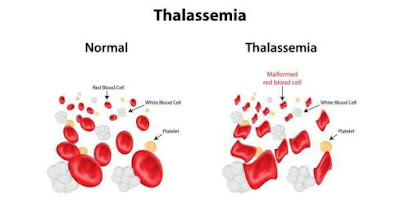
Diagnosis. Clues to the diagnosis of thalassemia trait is a mild anemia with a profound microcytosis. Beta thalassemia major has the severe symptoms, large spleen, and bone abnormalities described. Both forms of thalassemia are diagnosed by having a microcytic anemia with normal iron studies. Hemoglobin electrophoresis differentiates which type of thalassemia is present. In beta thalassemia, there is an increased level of hemoglobin F and hemoglobin A 2 . In beta thalassemia major, the hemoglobin is as low as 3–4 g/dL. Those with alpha thalassemia will have normal amounts of hemoglobins F and A 2 . Tetrads of beta chains are called hemoglobin H. Hemoglobin H is present in alpha thalassemia with 3 of 4 genes deleted. Target cells are present in all forms of thalassemia trait and thalassemia major. The RDW is normal in all forms because all of the cells are of the same size.
Treatment. Thalassemia traits of both the alpha and beta types do not require specific treatment. Beta thalassemia major patients require blood transfusions once or twice a month. The chronic transfusions lead to iron overload, which requires treatment with deferasirox. Oral deferasirox is the standard of care. This is easier to give than deferoxamine, which requires a subcutaneous pump. Splenectomy eliminates a major area of hemolysis and therefore helps reduce transfusion requirements. A small number of patients can be treated with a bone marrow transplantation