Difficult Airway Decision Pathways
Difficult Airway Decision Pathways
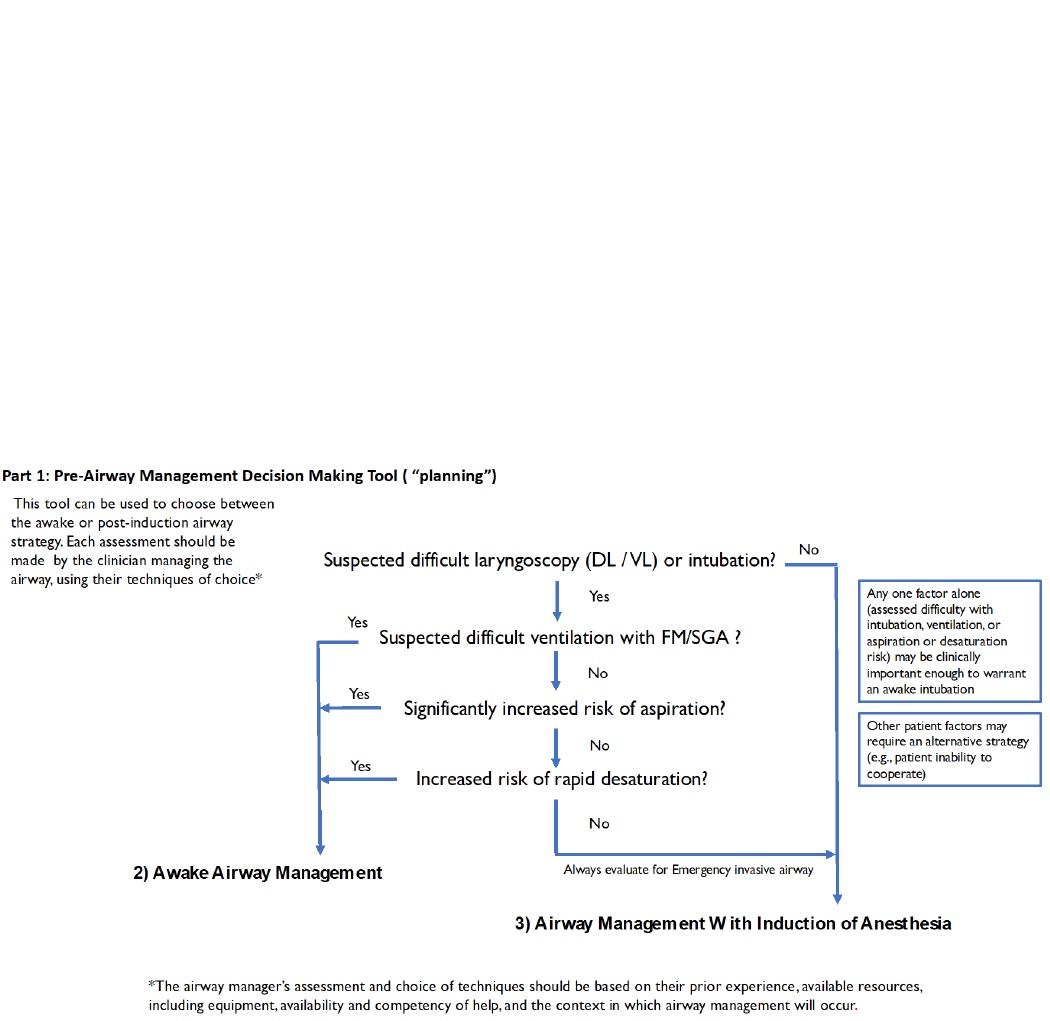
Part 1 is a decision tool that incorporates relevant elements of evaluation and is intended to assist in the decision to enter the Awake Airway Management or Airway Management with the Induction of Anesthesia arms of the ASA difficult airway algorithm.
Part 2 is an awake intubation algorithm:
Part 3 is a strategy for managing patients with induction of anesthesia when an unanticipated difficulty with ventilation with a planned airway technique (as determined by ) is encountered:
a Review airway strategy: consider anatomical / physiological airway difficulty risk, aspiration risk, infection risk, other exposure risk, equipment and monitoring check, role assignment, A/B/C back-up and rescue plans. Awake techniques include FIS, VL, DL, SGA, combined, retrograde-wire aided.
b Adequate ventilation by any means (e.g., FM, SGA, TI) confirmed by capnography when possible.
c The intent of limiting attempts at TI and SGA insertion is to reduce the risk of bleeding, edema, and other types of trauma that may increase the difficulty of mask ventilation and/or subsequent attempts to secure a definitive airway. Persistent attempts at any airway intervention, including ineffective mask ventilation, may delay obtaining an emergency invasive airway. A reasonable approach may be to limit attempts by any device to 3, with 1 additional attempt by a clinician with higher skills
d Optimize: suction, relaxants, repositioning, FM: oral/nasal airway, hand mask grip. SGA: size, design, repositioning, 1st vs 2nd gen. TT: introducer, rigid stylet, VL hyperangulated, blade size, external laryngeal manipulation. Consider other causes of inadequate ventilation (including but not limited to laryngospasm, bronchospasm)
e 1st vs 2nd generation SGA with intubation capability for initial or rescue SGA
f Video Laryngoscopy as an option for initial or rescue TI
g Invasive airways include: surgical cricothyrotomy, needle cricothyrotomy with a pressure regulated device, large bore cannula cricothyrotomy or surgical tracheostomy. Elective invasive airways include the above and retrograde wire guided intubation, and percutaneous tracheostomy. Other options include rigid bronchoscopy and Extracorporeal Membrane Oxygenation (ECMO)
h Follow-up care includes post-extubation care (i.e., steroids, racemic epinephrine), counseling, documentation, team debriefing, encourage patient difficult airway registry
i Postpone the case / intubation - Return with appropriate resources (e.g. personnel, equipment, patient preparation, awake intubation)
i Invasive airway is performed by an individual trained in invasive airway techniques, whenever possible.
k In an unstable situation, or when airway management is mandatory after a failed awake intubation, a switch to the Airway Management With Induction of Anesthesia pathway may be entered with preparations for an emergency invasive airway
l Low or High Flow NC, head elevated position throughout procedure. Non-invasive ventilation during pre-ox.
Source: 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway