Positive end-expiratory pressure: advantages and disadvantages
All modes will require setting positive end-expiratory pressure (PEEP). PEEP represents the lowest airway pressure
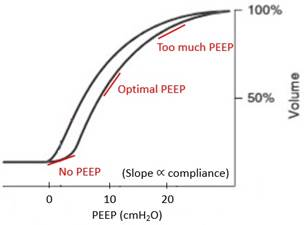
that the lung will be allowed to fall to on end exhalation. It is commonly misunderstood as pushing air back into the lung on exhalation, when in fact it is more akin to providing a bottom limit to the decline in airway pressure. PEEP allows more alveoli to remain open at the end of a breath. Over time the application of PEEP will lead to cyclical recruitment of alveoli and an improvement in oxygenation.PEEP improves oxygenation best in pathologic states that involve shunt from collapsed or filled alveoli such as pneumonia, ARDS, pulmonary edema, and atelectasis. Although increasing peak airway pressure and tidal volume can recruit lung on inspiration, the lung will derecruit again on exhalation. The cyclical opening and closing of alveoli is thought to be a key mechanism for ventilator-induced lung injury. PEEP on the other hand maintains alveolar recruitment and is a less injurious method of lung recruitment. Even patients with healthy lungs will benefit from a small amount of i-PEEP to prevent derecruitment during intubation. Five of PEEP is applied nearly universally.
PEEP can have adverse consequences especially at overly high levels. It can lead to hemodynamic impairment by decreasing RV preload. High alveolar pressures can lead to west zone 1 conditions (alveolar pressure exceeds capillary pressure), a regional fall in blood flow, and increase in dead space ventilation. High PEEP can lead to a global rise in pulmonary vascular resistance through this same mechanism and exacerbation of right heart dysfunction. PEEP can also cause overdistension and damage of normal alveolar segments especially when there is normal lung adjacent to un-recruitable consolidation.